Chickenpox symptoms, treatment and vulnerable groups

Key learning points
- Varicella is a usually mild illness mainly affecting children but carries a 30% mortality rate in infants under four weeks.
- Non-immune pregnant women are at high risk of complications for both themselves and the baby but the vaccine is contraindicated during pregnancy.
- The use of non-steroidal anti-inflammatory painkillers (NSAIDs), such as ibuprofen, is not recommended as this increases the risk of severe skin and soft tissue infections.
Varicella, more commonly known as chickenpox, is an acute childhood disease characterised by a vesicular rash, often preceded by fever and general malaise. Most children will catch it at some point. Its incidence is highest before the age of 10 years and peak incidence of varicella usually occurs from March to May, although in recent years there has been less seasonal variation.1 Adults are vulnerable to the disease if they did not have it as a child.
Symptoms
As this is a highly infectious disease, with up to 90% of susceptible contacts going on to develop it,2 diagnosis can often be made by a discussion with parents about siblings or close contact with others who have recently had the disease. Close contact is defined as five minutes face to face or 15 minutes in the same room.3 As there is a high risk to neonates and pregnant women, this discussion could take place over the phone to decrease the risk of them infecting vulnerable patients who may be attending the surgery. If facilities allow, you can suggest that parents send a photograph of the spots for confirmation.
Before the characteristic spots appear, children usually suffer general malaise, and can show the following symptoms:
- Feeling tired and generally unwell.
- Fever of 38°C or above.
- Nausea.
- Aching, painful muscles.
- Anorexia.
- Headache (particularly in adolescents).
These are the more common symptoms but younger children may not present with any of the above before the first spot appears. The incubation period can be as long as three weeks, so parents may be unprepared for siblings becoming unwell later. The length of incubation period can increase in children who are immunocompromised, so any vulnerable child will need to be carefully monitored in the event of close contact. Varicella is infectious from two days before the rash appears.
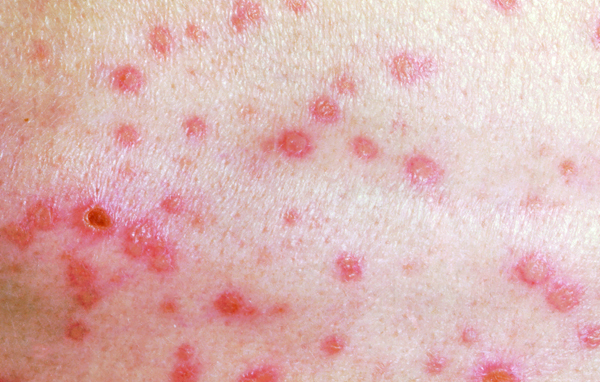
The rash
The chickenpox rash has three distinct phases.
- The rash starts as small erythematous macules on the scalp, face, trunk and proximal limbs, which very quickly develop (over a matter of hours) to papules, clear vesicles (which are intensely itchy) and then pustules.
- Vesicles appear in crops; stages of development can therefore differ on various areas of the body. Vesicles can also occur on the palms and soles, and even on mucous membranes, causing painful and shallow oral or genital ulcers.
- About five days after the first spots appear, the first vesicles begin to dry out and crust over. Once all the vesicles have crusted over, the child is no longer infectious and should be advised to return to school or nursery.
Phase 1

Phase 2

Related Article: Weight loss medication is no magic wand
Phase 3
Treatment
You should be aware of any community outbreaks. You can use this local knowledge to help deter otherwise well individuals from visiting the GP surgery for diagnosis and thereby decrease the risk to non-immune antenatal women, neonates and immunosuppressed patients. Practice nurses can give advice over the phone and community nurses, when visiting the elderly at home, should advise patients who are suffering from herpes zoster not to be in contact with any person who has not had varicella.
Most cases of varicella are mild and self-limiting, and can be treated at home, as complications in otherwise well individuals are rare.4
You may also need to explain to families that there is no cure or current routine vaccination in this country against varicella.
You should offer advice about hydration, pain relief and care of the skin.
In many cases, paracetamol can be prescribed if you hold the V100 prescribing qualification, although only for infants older than eight weeks. This may also be a good opportunity to emphasise the advice about not using ibuprofen.
Even if you do not issue a prescription yourself, the legislation and liability for the medication is the same as if you have issued a paper prescription.
You can also offer advice about other measures for the relief of the itchy spots to decrease the risk of a secondary bacterial skin infection and scarring. Simple measures, such as keeping nails short and clean, patting the skin instead of scratching and the use of cotton gloves (or socks over the hands) at night, are worth suggesting.
Moisturising creams, cooling gels and loose cotton clothing can all be helpful.
Calamine lotion is thought to relieve itch by evaporating from the skin to induce a cooling effect.5 But NICE clinical knowledge summary has found no evidence for this, and some experts even suggest that drying the skin with calamine can increase the itch.6 Similarly, there appears to be limited evidence to support the use of either topical or systemic antihistamines.7
You are also in the ideal situation to identify those who may be at higher risk of complications.
Complications can include:
- A secondary bacterial skin infection such as impetigo (manifested by a sudden high-grade pyrexia).
- Neurological complications.
- Myocarditis, appendicitis, pancreatitis or arthritis.
Vulnerable groups:
1. Adults
As with other childhood diseases, varicella can be more serious in adults. They are more likely to be admitted to hospital. Of the mortality related to varicella in England and Wales, 80% occurs in adults.2 Complications include pneumonia, hepatitis and encephalitis.
Smokers are at particular risk of developing fulminating varicella pneumonia.1
Shingles can occur from reactivation of latent varicella-zoster infection.
The National Institute for Health and Care Excellence (NICE) gives this advice on shingles:
- Explain that only a person who has not had chickenpox or the varicella vaccine can catch chickenpox from a person with shingles. The person with shingles is infectious until all the vesicles have crusted over (usually five to seven days after rash onset).
NICE also states that a person suffering from shingles should:
- Avoid contact with people who have not had varicella, particularly pregnant women, immunocompromised people and infants younger than one month of age.
- Avoid sharing clothes and towels.
- Wear loose-fitting clothes to reduce irritation.
- Cover lesions that are not under clothes while the rash is still weeping.
- Avoid use of topical creams and adhesive dressings, as they can cause irritation and delay rash healing.
- Keep the rash clean and dry to reduce the risk of bacterial super-infection. Seek medical advice if there is an increase in temperature, as this may indicate bacterial infection.
- Avoid work, school or day care if the rash is weeping and cannot be covered. If the lesions have dried or the rash is covered, these avoidances are not necessary.10
2. Antenatal women
Related Article: Prescribing in England to be led by a single national formulary
Pregnant women who catch varicella are at increased risk of varicella pneumonia and are far more likely to suffer a severe form of the disease. Around 10% of pregnant women with varicella develop pneumonia. The severity of illness is increased if the pregnancy is more advanced. Case fatality rates vary between 0-14%.2
Implications for the foetus:
- Infection before the 29th week of pregnancy can lead to intrauterine infection and foetal varicella syndrome. This can include skin scarring, eye defects, hypoplasia of the limbs and neurological abnormalities.
- If a pregnant woman contracts the disease one to four weeks before delivery, her newborn infant has up to a 50% chance of being infected, and about 25% of these infants will develop clinical varicella of the newborn.
- If the infant is born up to seven days before or seven days after onset of the mother’s rash, it is more likely to develop severe infection, which may be fatal.1
You need to be aware of this severe risk and follow the local policies. NICE advises to seek immediate specialist advice on further management.8
3. Breastfeeding women
A breastfeeding woman is more at risk of serious complications because she is an adult, but she also needs advice on contacts, as she may be more likely to be socialising with pregnant women, other breastfeeding women and neonates.
If she consults within 24 hours of developing the characteristic rash, best practice is to refer her to a medical prescriber. This is because the use of aciclovir medication has been shown to reduce the time to full crusting of the lesions and reduce the number of lesions if given early enough.9 Beware of asking her to attend the GP surgery in person, given the risk of contact with vulnerable patients.
Aciclovir is present in low concentrations in breast milk and should not adversely affect the infant. In addition, the health gains of breast milk for both mother and infant need to be reinforced, and mother and infant may experience difficulty getting back to full breastfeeding after an episode of varicella, if mother and infant have been separated or the infant given a breast milk substitute. If the mother is unfortunate enough to develop lesions near the nipple, show her how to hand express. The expressed breast milk can be fed to the infant if the infant is protected by the varicella-zoster immunoglobulin or aciclovir.10 NICE recommends a specialist should initiate these treatments.8 Self-care recommendations are the same as for other types of patient.
The author is a senior lecturer at a Baby Friendly accredited university, which supports the International Code of Marketing of Breastmilk substitutes. The Code does not allow any promotion of infant formula. The author has not accepted a fee for this article as this journal, like most nursing publications, is not code compliant.
References
1 Public Health England. Varicella. In: The green book. PHE 2015.
2 Royal College of Obstetricians & Gynecologists. Chickenpox in Pregnancy. RCOG 2015.
3 Johnson G. Minor illness in the under-fives. A guide for Health Visitors. USA Publishing 2015.
4 Lichenstein R. Pediatrics, chicken pox or varicella. WebMD 2006
Related Article: Advice on Guillain-Barré risk for adult RSV vaccine updated by MHRA
5 Allen S. Chickenpox and shingles infection. Pharmaceutical Journal 2006;277:453-6.
6 Acute varicella-zoster. British Medical Journal Best Practice 2016. bestpractice.bmj.com/
7 Gould D. Varicella zoster virus: chickenpox and shingles. Nursing Standard 2014;28:52-8.
8 NICE. CKS: chicken pox cks.nice.org.uk/chickenpox
9 Cohen J, Breuer J. Chickenpox: treatment. BMJ Clinical Evidence 2015
10 NICE. CKS: chicken pox, scenario 3 cks.nice.org.uk/shingles#!scenariorecommendation:3

See how our symptom tool can help you make better sense of patient presentations
Click here to search a symptom


Varicella, more commonly known as chickenpox, is an acute childhood disease characterised by a vesicular rash, often preceded by fever and general malaise. Most children will catch it at some point.



