Hydrocolloid dressings: the essential guide

Hydrocolloids have been available for clinical use for over 20 years. They were one of the first dressing types designed to apply the principles of moist wound healing.
Hydrocolloid dressings contain a gel-forming agent that has been applied to a carrier backing, such as a foam or film, to form a wafer that can be directly applied to a wound. The gel-forming agent will vary between products but is likely to include ingredients such as sodium carboxymethyl cellulose or gelatine. A gel is formed when the dressing comes into contact with wound exudate.
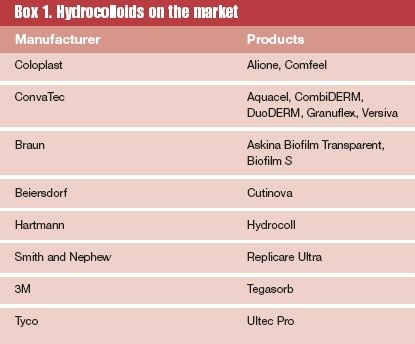
Although hydrocolloids are most commonly known as flat dressings, they are also available in a variety of contoured dressings (eg, elbow, sacrum and heel dressings) and as a paste filler. In the last few years, spun hydrocolloid dressings have also appeared on the market. These look very similar to alginates and share similar absorption and exudate management properties. Spun hydrocolloids require a secondary retention dressing -a hydrocolloid sheet is ideal.
Properties of a hydrocolloid
Most hydrocolloids are self-adhesive and impermeable to water vapour. Their occlusive nature means that moisture is retained at the wound bed. However, the dressing will become more and more permeable as gelling occurs, allowing the dressing to manage exudate through evaporation.
Related Article: Call for regulatory guidelines as NHS adopts AI in dermatology care
A hydrocolloid dressing will provide some degree of absorption of exudate but is unlikely to cope with copious exudate when maceration of the surrounding tissue may occur. Spun hydrocolloids are a more suitable option for managing heavy exudate.
Very recently, both flat hydrocolloid sheets and spun hydrocolloids have appeared in antimicrobial versions impregnated with slow-release silver. Silver is a broad spectrum antimicrobial that is believed to be effective in promoting healing in wounds by reducing the bacterial burden.
It is hoped that resistance will be less of an issue with silver than it is with topical antibiotic therapies. However, most companies manufacturing silver-impregnated dressings are currently recommending that silver dressings are usually effective in reducing the bacterial burden and restoring wound bed balance within four weeks. Therefore, for most patients, long-term use of silver is unnecessary and should be avoided on the basis of minimising the risk of resistance and silver toxicity and reducing cost.
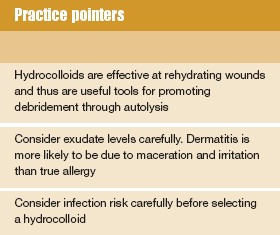
Instances of allergic contact dermatitis due to hydrocolloids are reported to be rare.(1) However, irritant contact dermatitis and maceration following inappropriate use is not unusual and may be mistaken for allergic contact dermatitis.
Different types of hydrocolloids
Because different brands use different gelling agents, hydrocolloids will differ between brands. Hydrocolloids are available in a wide variety of flat shapes. They are available with or without bevelled edges and adhesive borders, which increase wear time and comfort. Spun (or fibrous) hydrocolloids are available as both flat sheets and ribbon.
When to use a hydrocolloid
Selecting a dressing requires matching the characteristics of a product to the needs of the patient. Product characteristics will include its ability to conform to the contours of the body, handle fluid and odour, ease of application and removal with the attendant risks of pain and trauma, risk of causing sensitivity reactions and the frequency of dressing changes.
The needs of the patient may include the ability to self-care, shower or bathe, continence issues and sensitivity reactions. It is vital that any underlying conditions (eg, compression therapy for venous leg ulcers) are addressed in conjunction with dressing selection.
Cost-effectiveness should also be considered. However, this does not mean that the cheapest dressing should automatically be selected. The NICE guideline on debriding agents acknowledges that modern dressings, such as hydrocolloids, may reduce pain and be more acceptable to patients.(2) The guideline suggests that the selection of debriding agents should be based on impact on comfort, odour control and total costs, which should include consideration of dressing change frequency. Most hydrocolloid dressings can be left in situ for 3-5 days, and removal is usually pain-free.
The role of hydrocolloids in treating neuropathic wounds and arterially compromised wounds remains controversial. Some clinicians argue that the occlusive nature of hydrocolloids carries an increased risk of infection because of their effectiveness in rehydrating dry tissue. Others argue that rehydration and desloughing of dead tissue reduces the risk of infection. At the time of writing, no good evidence was found to guide clinical practice. It might be argued that hydrocolloids carry a risk for these groups of patients and should only be used with caution. The same rationale applies for patients with infected wounds.
Rehydration of necrotic tissue
When dead tissue remains in a moist environment (eg, within a pressure ulcer), separation from the underlying healthy tissue will usually happen spontaneously through autolysis. However, when dead tissue is exposed to a dry environment it will dehydrate, shrink and darken to form hard necrotic tissue.
In some situations, when underlying healing is unlikely (eg, arterially compromised toes) and rehydration would lead to an unacceptably high risk of infection (eg, some diabetic foot ulcers), it may be clinically preferable not to encourage rehydration. However, in many instances, rehydration and subsequent debridement through encouraging autolysis is the first step toward promoting healing.
Related Article: Abdominal body fat is a higher risk for developing psoriasis
Slough management
Slough is a yellow, glutinous covering that consists of protein, fibrin, exudate, leucocytes and bacteria. It can predispose a wound to infection since it forms an attractive medium for bacterial growth. Although a hydrocolloid dressing may encourage autolysis on a sloughy wound with minimal exudate, sloughy wounds often produce too much exudate for a hydrocolloid to handle without resulting in maceration of the surrounding skin.
Promotion of granulation
Pink/red granulation tissue is a highly vascular gel-like matrix that is contained within the fibrous collagen network. Although hydrocolloids are very effective for promoting granulation, their occlusive nature can sometimes result in overgranulation. This situation can often be resolved through the use of a dressing that is nonocclusive, which will moderate the hydration state of the wound bed.
Promoting epithelialisation
Epithelialisation tissue generally produces little exudate but is fragile and requires protection. Hydrocolloids can usefully fulfil this function.
Maggot therapy
Maggot therapy requires dressings that are able to prevent the maggots from escaping, provide sufficient oxygen and moisture, require minimal maintenance and be affordable. Suppliers of therapeutic maggots are currently recommending that hydrocolloid dressings be used to form an island dressing around the wound to protect the intact skin and provide a baseplate for a net covering to retain the maggots.
Pressure ulcers
The effectiveness of hydrocolloids for treating pressure ulcers will depend on an accurate assessment of the wound bed and level of exudate. However, a systematic review found evidence that hydrocolloid dressings are better than wet-to-dry dressings in treating pressure sores.(3)
Leg ulcers
In the treatment of venous leg ulcers, there is evidence to suggest that low adherent dressings (eg, knitted viscose) are as effective as hydrocolloid dressings beneath compression bandaging and have cost-effectiveness benefits.(3) However, hydrocolloids can be useful when it is evident that epithelialisation has successfully occurred under a scab (eg, the final healing stages of a leg ulcer). The application of a thin hydrocolloid to the wound bed can gently rehydrate and lift the scab, leaving intact epithelialisation tissue covering the wound bed.
To conclude, hydrocolloids were probably the first available modern dressings for many nurses. Many other types of products have since appeared on the market. However, manufacturers of hydrocolloids have continued to refine existing hydrocolloid dressings to increase their effectiveness and performance. In addition, manufacturers are continuing to develop new variations that harness the useful properties offered by hydrocolloids and incorporate new wound care technologies to increase the range of use for these products.
Related Article: CPD: Case by case – acute and emergency dermatology presentations
References
- Sasseville D, Tennstedt D, Lachapelle JM. Allergic contact dermatitis from hydrocolloid dressings. Am J Contact Dermat 1997;8:236-8.
- NICE Technology Appraisal No 24. Guidance on the use of debriding agents and specialist wound care clinics for difficult to heal surgical wounds. Available from: http://www.nice.org.uk/page.aspx?o=16583
- Bradley M, Cullum N, Nelson EA, et al. Systematic reviews of wound care management:(2) Dressings and topical agents used in the healing of chronic wounds. Health Technol Assessment 1999;3(17Pt 2):135. Available from: www.ncchta.org/
execsumm/summ3172.htm
Resources
The Cochrane Library
W:www.nelh.nhs.uk/cochrane
World Wide Wounds
W: www.worldwidewounds.com

See how our symptom tool can help you make better sense of patient presentations
Click here to search a symptom


A hydrocolloid dressing will provide some degree of absorption of exudate but is unlikely to cope with copious exudate when maceration of the surrounding tissue may occur.



