Mythbusters is a series of articles in which nurses tackle some of the common misconceptions that patients often present with, and advise how to debunk them during your consultation
The myth
Antibiotics are always required to treat fungal nail infections.
The reality
The appearance of an infected nail (yellow discolouration) and inflamed surrounding skin may lead a patient to believe that an antibiotic is necessary. They may not be aware that viral and fungal infections can require different management approaches, and that antibiotics are not appropriate unless there is a concomitant bacterial infection. It is important for nurses to dispel this myth by providing clear information and explanations about the patient’s type of infection, cause, treatment and management including self-help strategies.
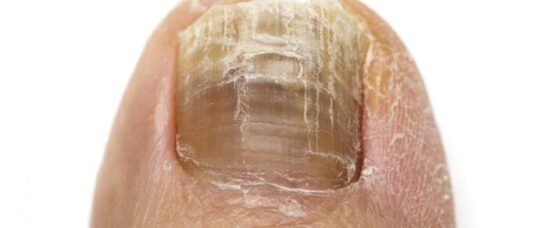
Fungal infections of the nails (onychomycosis) develop over time. They are more common in older patients and rarely affect children.
Generally, toenails are more commonly affected, with the infection involving any part of the nail unit, including the nail plate, nail bed and the root.1
When a patient presents with a skin problem or nail problem, it is important to take a comprehensive history and perform a skin assessment. The skin often provides vital clues, which can be missed if you look at lesions or presenting skin problems, including the nails, in isolation.
Patients may be shocked if, when showing you their toenails, they are asked to show other parts of their skin in more detail. However, this is important to do. If they have a fungal nail infection they may also have other concomitant fungal infections, such as: foot (tinea pedis), groin (tinea cruris), body (tinea corporis), hand (tinea manuum) and scalp (tinea capitis).
To establish and confirm the diagnosis of a fungal nail infection, the clinical assessment should also include taking a sample. Suitable samples include nail clippings or skin scraped from under
a nail for microscopy and culture (mycology). These will identify the fungus or other infective cause such as a mould or yeast.2
Dermatophyte fungi are the ringworm fungi (tinea) and are spread by direct contact from other people (anthropophilic organisms), animals (zoophilic organisms), and soil (geophilic organisms), and also indirectly from inanimate objects including upholstery, hairbrushes and hats.3
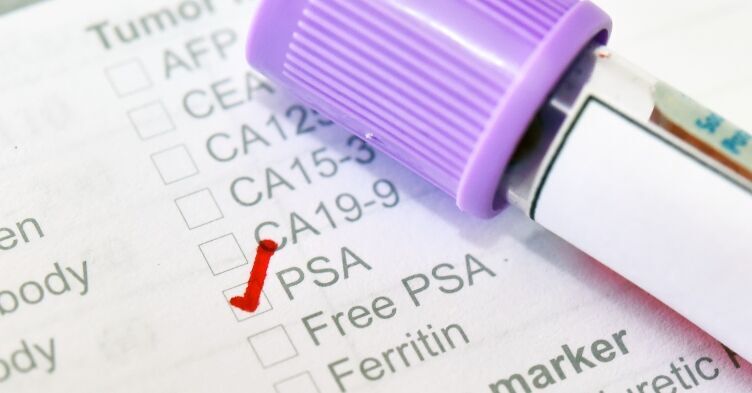
The next step is considering treatment options. Antifungals are used differently from antibiotics, which are usually given for a definitive time. Antifungal treatments require patients to commit to longer treatment regimens, which may include topical applications or oral medications.
The pros and cons should be reviewed and discussed with patients, as not everyone requires treatment and simple self-care measures may be appropriate and should be supported with written information about the infection.4
Self-care measures include minimising exposure to warm, damp conditions, not wearing occlusive footwear and avoiding trauma to the nails. The nails should be kept short and filed down. A podiatrist may be required if the nails are thickened and are affecting walking. Hygiene measures should be addressed, including treating any tinea pedis, wearing clean shower shoes in communal areas and not sharing footwear or equipment.1
References
1 NICE CKS. Fungal nail infection. London: NICE; 2014 cks.nice.org.uk/fungal-nail-infection#!scenario
2 Oakley A. Laboratory tests for fungal infections. Hamilton: DermNetNZ; 2003 dermnetnz.org/topics/laboratory-tests-for-fungal-infection/
3 Hainer B. Dermatophyte infections. Am Fam Physician 2003;63:101-8
4 British Association of Dermatologists. Patient information: fungal nail infections. London: BAD; 2017 bad.org.uk/shared/get-file.ashx?id=205&itemtype=document