Mythbuster: ‘IUDs are only for women who’ve had babies’
An intrauterine device, or IUD, is often referred to as a ‘non-hormonal coil’ or a ‘copper coil’. They last between five and 10 years, depending on which coil is fitted (usually decided by the size of the womb during the fit). IUDs are also the most effective form of emergency contraception and can be fitted up to five days after the expected ovulation date in any cycle.1
Another type of coil, an intrauterine system (IUS) or ‘hormonal coil’, can last between three and five years. These contain a hormone that releases into the uterus and acts on the lining, making periods lighter. This is useful if your patient has heavy periods, and is especially helpful if she is young and prone to being anaemic. It can also stop the lining forming at all so the woman has no periods.
Related Article: Prescribing in England to be led by a single national formulary
There is no age limit for having intrauterine contraception (IUC) and many young women, especially if they’ve tried the pill or a contraceptive injection, like the fact that they can have really effective contraception with fewer or no hormones. Both types are effective and prevent about 99.5% of pregnancies – this means that in 100 women using an IUC method for contraception a year, 0.5% will get pregnant (or, more simply, one woman in two years). Compare this with the pill, where nine out of 100 will get pregnant (or 18 in two years). All contraceptive pills contain a small amount of lactose, which is something to consider when advising women who are lactose intolerant or vegan.
Many women who are perimenopausal choose an IUS to reduce their bleeding, but young women can really suffer with heavy periods, which can impact their daily lives. NICE guidance on heavy menstrual bleeding3 recommends an IUS regardless of age, so if a young woman is struggling with periods and missing school as a result, or if heavy periods are impacting her ability to do an activity, an IUS can help her get her life back. Lots of young women choose to be fitted with one before heading off to university or going travelling.
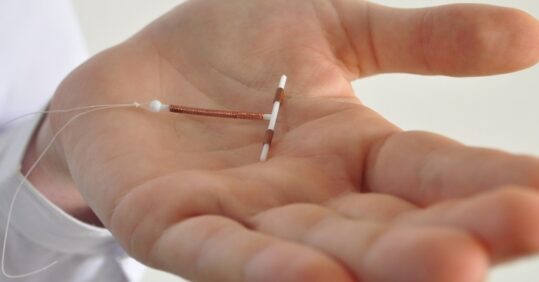
An IUD/IUS should be fitted by a specially trained nurse or doctor. If there isn’t a specialist at your practice, provide women with details of the local sexual health clinic and information on how to get a referral. Have a sample device handy, as actually seeing an IUD or IUS – a small T-shaped device, roughly the size of a 50p coin – can assuage a lot of worries. If you want more help on how to ‘sell’ IUCs to women, there is a free online course on contraception counselling you can do, hosted by the Faculty of Sexual and Reproductive Healthcare.2 You could always ask to shadow an experienced sexual health nurse to learn some tips.
An IUD must always be offered if a woman comes for emergency contraception, as it is the most effective type and also provides immediate ongoing contraception. If a woman decides she does not want an IUD fitted, she needs to be aware that oral contraception is second best, and you should always record that you have told her this.
Related Article: Advice on Guillain-Barré risk for adult RSV vaccine updated by MHRA
Most sexual health clinics provide drop-in appointments for women needing emergency contraception and can sort out the IUD fit, but your guidance will make all the difference to her actually going straight there. There is a lot of misinformation about IUDs and women often don’t know the facts. Many might have been told by their mum or other female relatives or friends that an IUD can only be fitted in women who have given birth – this may be ‘old’ medical advice they themselves were once given by a GP.
Remember to counsel your patient and explain: yes, she can have pain relief; yes, she is fertile immediately after a coil is removed; yes, she can have an IUD regardless of whether she’s had a baby; no, neither she nor her partner will feel it during sex. Also, make sure you encourage women to check the threads so they learn what is normal, especially after removing tampons or a menstrual cup. Suggest they keep a record of their periods using an app or a diary. IUDs and IUSs can be life changing, so find out the facts and make sure you’re counselling women about the benefits.
Eppy Sewell is a specialist nurse in contraception in Buckinghamshire and a peripatetic IUC trainer
Related Article: Quick quiz: Management of COPD
References
- fsrh.org/standards-and-guidance/documents/ceuguidanceintrauterinecontraception
- fsrh.org/education-and-training/fsrh-contra-ceptivecounselling-online-course
- nice.org.uk/guidance/ng88

See how our symptom tool can help you make better sense of patient presentations
Click here to search a symptom


Women’s health specialist nurse Eppy Sewell on how the coil can be life-changing for younger women



