CPD module: Intrauterine contraception – what practice nurses need to know
Nurse specialist in sexual health and contraception Jodie Crossman outlines the main forms of intrauterine contraception, their appropriate use and best practice in advising patients
Intrauterine contraception (IUC) is one of the oldest methods available to people with a uterus who want to prevent pregnancy. It is highly effective, with less than 1% of users of IUC becoming pregnant.
This learning module will enable you to understand the different types of intrauterine contraception, advise patients and prepare them for fitting, and understand risks and problems that can occur.
Related Article: ‘Concerning acceleration’ in drug-resistant gonorrhoea ahead of vaccine programme
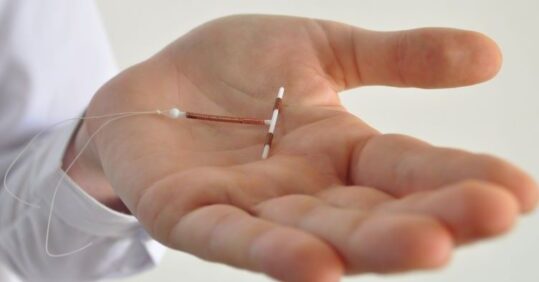
Commonly referred to as ‘the coil’, IUC comes in two different forms:
- Intrauterine Device (IUD), also known as the copper coil
- Intrauterine System (IUS), also known as the hormonal coil
The fitting of both types of coil is the same, but their mechanism of action is different.
The IUD is a T-shaped device which is wrapped with very thin copper threads. Its primary mechanism is providing an inhospitable environment for fertilisation, as copper is toxic to sperm and ova. In addition, the copper provokes changes in the cervical mucus, which can inhibit sperm penetration. It also causes an inflammatory effect which, if fertilisation has already occurred, prevents implantation.
The IUS looks similar to the IUD, but has an elastomer core which slowly releases the progestogen hormone levonorgestrel (LNG). In addition to an inflammatory effect, the IUS has a progestogenic effect on the endometrium, thinning the lining to make implantation difficult, and increasing the presence of phagocytic cells to prevent sperm reaching an egg.
As there are no changes to the natural cycle, and no hormonal side effects, the IUD may be an ideal method for people wanting ‘fit and forget’ methods, such as those who have tried hormonal contraception and found the side effects intolerable, or would like to maintain their regular cycle, or who cannot use hormones for other reasons (for example, trans men who are concerned about effects of hormones on their transition).
Although any appropriately trained health professional can offer contraceptive counselling, clinicians fitting IUC should hold the appropriate Faculty of Sexual and Reproductive Health (FSRH) Letter of Competence in Intrauterine Techniques (or equivalent competencies).
Related Article: Action needed to tackle untreated hearing loss in care homes
Key points
- Before fitting a coil, a medical history should be taken, including a full gynaecological, contraceptive and obstetric history
- A sexual history is also important, and chlamydia and gonorrhoea testing should be offered to all people
- IUC should not be fitted if there is a risk of established pregnancy, if unexplained vaginal bleeding is a current issue, or if the patient is symptomatic of PID
- Once suitability for IUC is established, patients should be advised about the fitting procedure
- Immediately after IUC fitting, patients should be monitored for signs of vasovagal response
Author
Jodie Crossman is Nurse Team Leader at Brighton and Hove Sexual Health and Contraception Service and is chair of the British Association of Sexual Health and HIV Nurses and Health Adviser group.
Find this learning module
Related Article: Government to introduce HPV self-sampling for ‘under-screened’ women
The full module can be found on the Nursing in Practice website.
Not a Nursing in Practice Learning member? Click here to register for free and gain access to more CPD modules.

See how our symptom tool can help you make better sense of patient presentations
Click here to search a symptom




