Supporting access to intrauterine contraception
Nurse specialist in sexual health and the menopause Ruth Bailey provides an update on current recommendations for use and fitting of intrauterine contraception
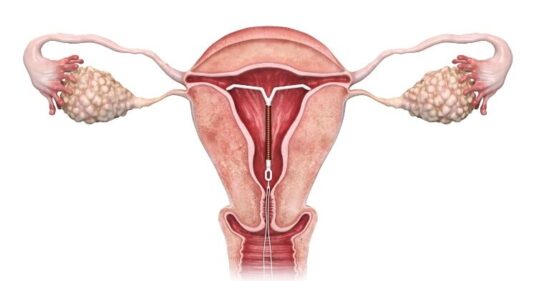
Intrauterine contraception (IUC) – also known as the coil – is a type of long-acting reversible contraception (LARC) which has been shown to be one of the most effective methods in reducing the risk of unplanned pregnancy.1
There are two types of IUC available in the UK – the copper intrauterine devices (Cu-IUDs) and levonorgestrel intrauterine devices (LNG-IUDs). They are equally effective, but work in different ways, and have different side effect profiles, so it is important that patients are counselled on these, so that they can select a method that best suits their needs.
A number of changes have been made to the Faculty of Sexual and Reproductive Healthcare (FSRH) guidance on use of IUC in quick succession (see Box 1). This article provides a summary of the updated guidance recommendations, to enable practice nurses to provide up to date information to support patients with their contraceptive choices.
Box 1. Summary of key FSRH guidance updates
- In March 2023 the FSRH updated its clinical guidance on the use of IUC to reflect new evidence. Shortly afterwards, in July 2023, the guidance was amended to reflect changes to the duration of use for 52 mg levonorgestrel intrauterine devices (52 mg LNG-IUDs).2
- In January 2024, the licence for the Mirena 52 mg LNG-IUD changed, extending its use from 5 to 8 years for contraception.
- Then in May 2024, the FSRH published a further statement announcing that use of any 52 mg LNG-IUD for contraception could be extended to 8 years (noting 8 years is off-label for Levosert or Benilexa).3
Copper intrauterine device (Cu-IUD)
The Cu-IUD is a non-hormonal contraceptive device that works by inhibiting fertilisation through the effect of copper on sperm. It causes an inflammatory effect on the lining of the womb and can make periods heavier and longer. It is a good contraceptive choice for women who have experienced side effects with hormonal methods or who simply prefer to avoid hormones.
The copper coil works immediately after it is inserted into the womb. It can last between 5-10 years depending on its type and licence. The FSRH supports extended use of the copper coil fitted in women aged 40 and over until the menopause provided the Cu-IUD contains ≥300mm2 of copper.4
The Cu-IUD is the most effective type of emergency contraception, provided it is fitted within 120 hours of unprotected sexual intercourse (UPSI) or within 5 days of expected ovulation and that there is no risk of pregnancy from UPSI earlier in the cycle.5
Nurses have a key role in advising women on their choices for emergency contraception and accessing appointments, so it is important to be aware of local pathways.
Levonorgestrel intrauterine device (LNG-IUD)
LNG-IUDs are hormonal coils that work primarily by changing the cervical mucous to make it impenetrable by sperm, and by thinning the endometrium (womb lining) to inhibit implantation. This suppresses ovulation in some women, although this is not the main action of LNG-IUDs.
There are currently five types of LNG-IUD available in the UK, and these are summarised in Table 1 below.
Related Article: Postnatal contraception advice reduces the risk of back-to-back pregnancies
The LNG-IUD can be fitted at any time in the cycle if pregnancy has been excluded and no unprotected sex has taken place since the last period.
If fitted on days 1 to 5 of the natural cycle, the device will be effective immediately, if fitted later in the cycle then extra precautions will be required for 7 days unless the woman is switching from reliable use of another method.5
Beneilexa, Levosert and Mirena – 52 mg LNG-IUDs
Benilexa, Levosert and Mirena all contain 52 mg of levonorgestrel. New FSRH guidance supports their use for contraception for 8 years, if fitted for women aged 45 and younger.3 If fitted over the age of 45, they may stay in place until menopause or age 55, after which time contraception is not required.4
All 52 mg LNG-IUDs are supported by both the British Menopause Society (BMS) and the FSRH to be used as endometrial protection for women receiving oestrogen hormone replacement therapy (HRT) for 5 years. However, it is only the Mirena which is licenced for this use and the licence is for 4 years, so use for 5 years remains unlicenced.6
Women using a 52 mg LNG-IUD for both contraception and HRT will need to have their coil changed at 5 years to provide sufficient endometrial protection, so it is important to ensure that the patient knows when their coil should be changed and that this is clearly documented in the patient record.
The 52 mg LNG-IUD is an extremely effective treatment of heavy menstrual bleeding (HMB) because of the effect of levonorgestrel on the endometrium. Both the Mirena and Levosert IUDs are licenced to be used for HMB for 5 years and Benilexa is licenced to be used for HMB for 3 years.
Women frequently use the coil for both contraception and to manage HMB and so the coil may need to be changed earlier than 8 years, and the appropriate timing should be assessed individually based on symptoms and the women’s preference.
Kyleena – 19.5 mg LNG-IUD
The Kyleena LNG-IUD contains less levonorgestrel, and although it will thin the endometrium and significantly reduce blood flow, it is not suitable for treatment for HMB and not licenced for use as endometrial protection as part of HRT. It remains highly effective contraception for 5 years and its reduced dose of levonorgestrel means that it is a good choice for women who have experienced hormonal side effects in the past.
The width of the fitting device is smaller than 52 mg LNG-IUD so it can be fitted comfortably for women who have a small os.
Jaydess – 13.5 mg LNG-IUD
The Jaydess LNG-IUD has the lowest dose of levonorgestrel and is licenced for use for 3 years. It is the same size as a Kyleena, which has largely replaced the Jaydess, as it is effective for a further 2 years. Although not currently being promoted, it is still available, and some women prefer to continue with its use as it offers the lowest dose of hormone.
The role of the general practice nurse (GPN)
GPNs play a pivotal role in promoting and providing IUDs for contraception, HMB and as part of HRT.7 Many myths and misconceptions about the use of IUDs exist, and a skilled consultation that provides clear explanations and evidence-based information is vital in supporting patient choice.
Nurses should be conversant in the UK medical eligibility criteria to exclude current pregnancy, assess the patient and make sure they meet the criteria to benefit from the method.8
A medical and sexual history should be taken, cervical screening discussed if the patient is eligible, and sexual health screening should be offered. FSRH guidance states that the risk of sexually transmitted infections should be assessed, and screening carried out if appropriate. This can be carried out at the time of the fit, if the clinician is confident that they could contact the patient for treatment if required.2 Patients should be advised on the timing of the procedure and offered contraceptive choices to avoid UPSI which would delay the fit until pregnancy could be excluded.
It is important the patients are fully counselled on risks, benefits, and side effects to ensure informed choice. The discussion and verbal consent should be recorded in the patient record as written consent is no longer required. Good preparation can greatly enhance the patient experience, and so time taken to prepare the patient, explain the fitting procedure and advise on pain management options is essential.
After-care
Routine follow-up after a coil fit is not required. However, patients should be taught how to check their coil threads and be advised to arrange a follow-up appointment if they are unable to do this. They should also be advised to make an appointment if they have pain that doesn’t settle with over-the-counter painkillers, or they experience heavy bleeding or fever, as these symptoms may indicate infection or perforation.
Related Article: ‘Concerning acceleration’ in drug-resistant gonorrhoea ahead of vaccine programme
IUD removal
Patients are often reassured if they know that the IUD can be removed easily, in case they have any difficulties with the method or decide to plan a pregnancy. They should be advised that unless planning a pregnancy, they should avoid UPSI in the 7 days before the procedure.
The coil can be removed by any registered nurse who is trained in the method and competent to do so – they do not have to be a coil fitter to carry out the procedure. The FSRH website has training videos on how to remove IUDs.
GPNs who are interested in extended their skills to gain accreditation for IUD fitting can do so through the FSRH (see Box 2).
Box 2. Extending skills – IUD fitting
Fitting and removing LARCs is an extremely rewarding role. It extends access to LARCs and offers continuity of care for patients that can be very reassuring.
GPNs who want to gain accreditation as a coil fitter can access the FSRH intrauterine contraception Letter of Competence (LOC) if they have a current FSRH Diploma (DFSRH) or have successfully completed the FSRH online theoretical assessment (OTA) and completed the relevant NHS England e-Learning for Healthcare modules.
Trainees will need to have an appointed Faculty Registered Trainer and protected time to complete coil training clinics. Details of local trainers may be found on the FSRH website or may be accessible through product manufacturers.
Access to safe and reliable contraception is a fundamental human right and an essential component of women’s health. GPNs are well placed to facilitate access to intrauterine contraception, to prevent unplanned pregnancy, to manage HMB and to provide endometrial protection as part of HRT, through careful assessment, and providing advice and information based upon the latest evidence.
Ruth Bailey is an ANP in sexual health, BMS accredited menopause specialist, Queen’s Nurse, Chair, RCN Women’s Health Forum and FSRH Council Nurse Rep
References
- Long-acting reversible contraception. CG30. 2019
- Clinical Guideline: Intrauterine contraception (March 2023, Amended July 2023)
- CEU Statement: Extended use of all 52mg LNG-IUDs for up to eight years for contraception. May 2024
- 2017a. Clinical Guideline: Contraception for Women Aged over 40 Years (August 2017, amended July 2023)
- 2017b. Clinical Guideline: Emergency Contraception (March 2017, amended July 2023)
- British Menopause Society. Management of unscheduled bleeding on hormone replacement therapy. 2024
- Jones E. Promoting the use of long-acting reversible contraceptives to reduce unplanned pregnancies. Primary Health Care; Published online 16 August 2023
- UK Medical Eligibility criteria Summary Sheet (April 2016, Amended September 2019)
Useful websites
Related Article: Government to introduce HPV self-sampling for ‘under-screened’ women
British Menopause Society www.thebms.org.uk
Contraception Choices www.contraceptionchoices.org
Faculty of Sexual and Reproductive Healthcare www.fsrh.org
Primary Care Women’s Health Forum (pcwhf.co.uk)
Sexual health education directory | Public Health | Royal College of Nursing

See how our symptom tool can help you make better sense of patient presentations
Click here to search a symptom




