How to develop the nursing care home workforce

Louise Brady outlines how the Royal British Legion is working to support care home nurses and carers, and develop its workforce, amid the challenges facing the whole sector.
Those who work within care homes have much to be proud of with dedicated and committed staff providing care that can transform the lives of those they work with. It is without question that UK care homes are at the frontline of health and social care provision today, managing the complex and critical needs of our older populations. In England alone, the provider workforce employs approximately 670,000 people, caring for just under 400,000 older people who have complex health and social care requirements (Skills for Care, 2017). Compelling evidence of why care homes are not only integral to our older citizens and their families, but also to the wider economic wellbeing of our workforce and communities, has come into sharp focus during the Covid-19 pandemic.
Workforce knowledge gap: registered nursing workforce
For registered nurses working within social care, the diversity of organisational approaches to policy practice and education are of great importance. Who employs the nursing care home workforce, what conditions do they work under, and what are the opportunities to develop established career pathways to support recruitment, retention and career development?
With an increasingly ageing population, the critical requirement for high‐quality care provision is set to rise and will require the employment of nursing staff with the breath depth and complexity of nursing knowledge, skills and values. However, the care sector is facing a staffing crisis. Registered nurses working within the NHS earn 7% more than those working in adult social care, which is partly responsible for the gap as deduced by a Health Foundation report (2019).
Related Article: BREAKING: Nurses to staff neighbourhood health centres under 10-year plan
A discussion paper led by the National Care Forum in 2016, in conjunction with Skills for Care, addresses the many complexities facing Britain’s care home nurses today. It highlights the poor image of nursing in social care and addresses the need for education and continuous professional development opportunities, coupled with the importance of robust culture and management support. Care home nursing is a multi-faceted role – but it is unclear since the advent of the NHS Long Term Plan (2019) how integrated work has progressed in terms of system-wide workforce plans in partnership with the provider sector, with a particular emphasis on multi-disciplinary and interdisciplinary teams supporting their populations.
The focus on mental health, community and primary care workforce provision was much welcomed by the ambitions of the Long Term Plan. However, as the Health Foundation report illustrates, much of the development of the wider workforce progress relies heavily upon the provision and sustainability of the adult social care workforce. There is an abundance of literature reviews by charities such as the King’s Fund and other organisations that support this concept, but little emphasis and priority is given to the care home sector specifically, and no emphasis on the critical safety role of the nursing workforce mentioned in wider MDT strategies (The Academy of Medical Royal Colleges, 2020).
Royal British Legion: comprehensive strategy to support nurses and carers
The Government’s ‘A Vision for Adult Social Care: Capable Communities and Active Citizens’ as far back as 2010 emphasised that everyone has an important part to play in taking forward a workforce reform programme. It acknowledges that delivering this vision will demand a confident, capable and well-trained workforce that empowers people to have independence and choice, and enables them to stay healthy and active in the ways that the universal personalised comprehensive care agenda demands (2019).
With that in mind, the Royal British Legion, as a small care home provider, has developed a comprehensive learning and development framework. It has a defined career pathway to support the nursing and care workforce across their six care homes from ‘carer to consultant’.
The Royal British Legion homes are spread wide across the UK. Each has a local practice development facilitator dedicated to the continuous learning development and training of its nursing staff and carers within each locality, to enable local implementation in partnership with each home, its residents and its wider MDT.
The strategy is entitled ‘Recognise, Rethink, Remodel and Remember’ and is designed to support each stage of nurse and carer workforce development. It will work with staff and its beneficiaries to model ways that support and enhance local and practical implementation, based on an analysis of each home’s capabilities, their workforce profiles, and the necessary future skills required for development.
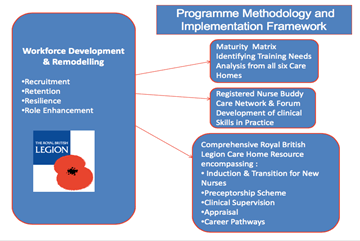
Preceptorship framework
A locally developed resource has also been made available for our care homes across the UK to support the practice and competency of newly registered nurses, those returning to practice and the new nursing associate role working within the care sector. It has been designed to facilitate induction, to accelerate career pathway development for nurses and carers new to social care, and to make the transition from learner to autonomous practitioner. Our preceptorship framework will align with existing evidence-based practice and ensure an operating model that aligns with Health Education England’s preceptorship standards (2015). In the acquisition and development of skills, as central to the development of a preceptorship programme, Patricia Benner’s novice to expert model will be used by preceptors to assess clinical competency, and proficiency.
Related Article: New ‘first-of-its-kind’ adult social care nursing faculty
Supporting people-powered care
As part of the programme, new staff are asked to connect with our residents to find out about their social history as a critical part of care planning. Finding out about veterans service history as a preceptee is a core component of the programme to optimise the therapeutic relationship between staff their families and their careers. Preferred forms of address, important memories, friendships, family service and social history are integral to care (Universal Personalised Care 2019).
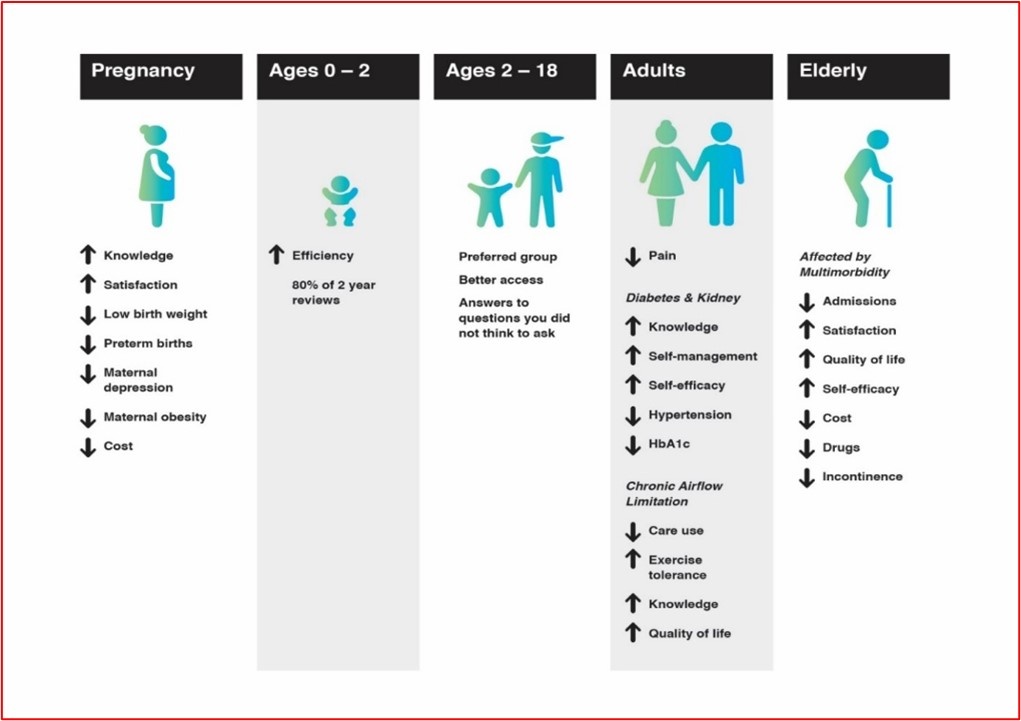
Care homes: Supporting long-term conditions and multimorbidity
The care workforce is facing enormous pressure to deliver high-quality care outcomes in diminishing time frames, against a backdrop of a depleting care workforce. A bio-psycho-social care model offering clinics embedded with care homes with support from the wider MDT is a model of care we are exploring in partnership with home managers, carers and our admiral nursing service. Within social care, group care can facilitate the delivery of the long plan goals by:
- Supporting early intervention
- Cohesive care planning with involvement from carers with older populations with multimorbidity
- Caring for staff
- Enabling better recruitment and retention of staff
The Royal British Legion’s ambition is to co-produce a social model of care in partnership with residents’ homes and families. Below is an example of the Art of the Possible:
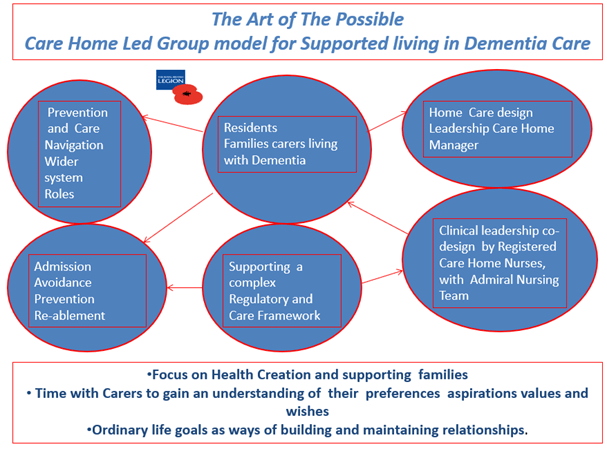
In groups the wider MDT – inclusive of nurses, carers, AHP’s residents’ families and volunteers – can realise workforce capacity and support proactive holistic care. It is a model that already provides a powerful way to integrate social, community primary and specialist care services (GP Forward View, 2016).
Related Article: QICN bids farewell to Dr Crystal Oldman as she retires from CEO role
Collaboration is key
Recruitment and retention of the nursing and care home workforce will be one of the most pressing challenges of the 21st Century. The value of the nursing and care workforce has been fully exemplified in the rapid advances we have seen during the Covid-19 pandemic. The social care workforce has kept their many residents safe and has stepped up to the incredible challenges they have faced.
However, collaborative working across boundaries and in partnership with multidisciplinary teams (MDTs) is a pressing concern. We now need to deliver a holistic comprehensive effective service enabling all parts of the care workforce, and importantly our nursing workforce has never been more relevant partners in this pursuit.

See how our symptom tool can help you make better sense of patient presentations
Click here to search a symptom




