Taking the temperature of practice nursing

Practice nursing has a recruitment and retention problem, but is it any wonder when the current cohort feels so undervalued?
In 2016, the General Practice Forward View announced a £15m fund to improve the ‘training capacity’ of nurses in general practice and ‘measures to improve retention’.
It was desperately needed – around half of the current practice nurse workforce is over the age of 50 and close to retirement. A 2016 poll by the Queen’s Nursing Institute found that around one in three nurses over 50 plan to retire by 2020.
 But the ideas surrounding improving retention were vague. The general practice nursing (GPN) ten-point plan mentioned ‘clinical supervision for nurses in general practice’ and implementing a ‘GPN career framework’, but with nothing fleshed out as to how NHS England or Health Education England would go about it.
But the ideas surrounding improving retention were vague. The general practice nursing (GPN) ten-point plan mentioned ‘clinical supervision for nurses in general practice’ and implementing a ‘GPN career framework’, but with nothing fleshed out as to how NHS England or Health Education England would go about it.
The outgoing chief nursing officer for England, Professor Jane Cummings, told Nursing in Practice last year that the ten-point plan will focus on ‘working with GP practices to explore flexibility within roles to improve retention and career development’.
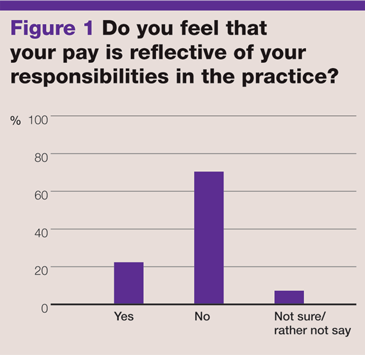
Yet our survey of 318 practice nurses found that, far from a lack of flexibility, the majority feel that their salary doesn’t reflect the responsibilities they hold at their practice.
Related Article: NHS 10-year plan: What does it mean for nursing?
When asked, 70% of the respondents didn’t feel that what they earned matched the work they undertook, with many reporting that they have upskilled in their own time and at their own cost with little reward (see figure 1).
‘I qualified as a nurse prescriber in 2011,’ one nurse told us. ‘But I have never had a rise in salary and I earn the same as my colleague who is not a prescriber’.
Another reported that she now fits implants as well as prescribing, but that no financial increment had been given to recognise the extra skill and responsibility.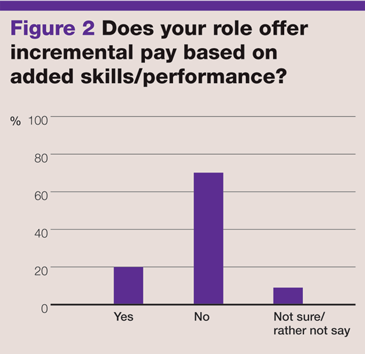
An almost identical number of respondents reported that their role does not offer incremental pay based on added skills (see figure 2). One nurse reported that she was told increments based on skills were offered at interview, only to find out later from her colleagues that this was not the case.
We were also told by a respondent that she was offered a pay rise upon completion of a prescribing course, but their practice refused to honour the agreement after the course was finished.
The ten-point plan does have a fleeting mention of a ‘model employment contract’ for GPNs, but the Royal College of Nursing (RCN) believes GP practices should be using Agenda for Change (AfC) contracts.
Josie Irwin, RCN’s associate director of employment relations, said: ‘The RCN has recommended that GP practices use AfC pay scales and terms and conditions since they were introduced in 2004. But GPs are private contractors with the NHS, which makes the enforcement of AfC pay scales difficult, and it is also unclear which NHS organisation would enforce these terms.
‘A substantial number of GP practices do mirror the AfC scales and therefore pay increments. Pay increments are designed to encourage development of skills and competence. Some GP practices pay spot rates based on an AfC pay band, but this is often the middle or even the bottom pay point of AfC.’
 The thorny issue of pay
The thorny issue of pay
As most practice nurses are not on AfC contracts, they do not benefit from the recent pay deal agreement. It means they are left at the mercy of individual practices.
Related Article: Nursing in Practice launches ‘How Nurses Count’ campaign
Of the 266 practice nurses who gave salary details, the average income per annum was £35,475, but this included gross salaries lower than £22,000 – below the starting salary for a newly-qualified band 5 nurse.
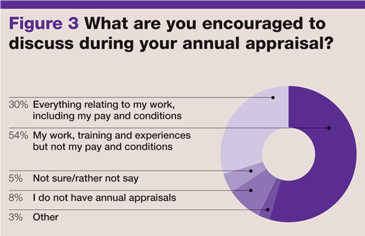
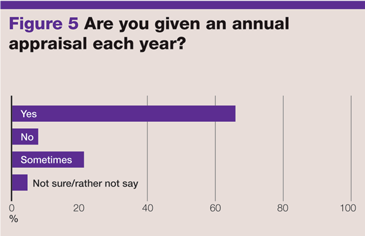
But when asking for a pay rise, more than half say they are not allowed to bring the issue up during their appraisal. Just under a third said they were allowed to discuss pay during their appraisal, with 8% claiming that they do not have annual appraisals at all (see figure 3).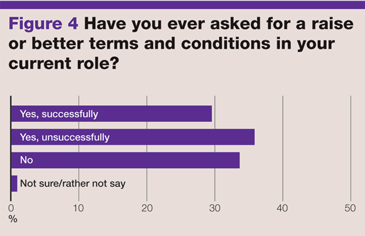
Reasons given to nurses for this varied from practices claiming that pay discussions ‘aren’t what appraisals are for’, or that they ‘cannot afford’ a pay rise, to those who ‘got in trouble’ for simply asking the question.
Ms Irwin agrees that an appraisal is not the time to discuss pay, and instead practice nurses should arrange a separate meeting to talk about remuneration.
She said: ‘A good appraisal will be about discussing past performance and considering development for the future, not a pay negotiation. A separate meeting with the employer to discuss pay should be arranged if the nurse feels they are underpaid or undervalued.’
 Less than a third of our respondents received a pay rise after asking. The remainder either asked and were rejected (35%) or didn’t ask at all (33%) (see figures 4 and 6).
Less than a third of our respondents received a pay rise after asking. The remainder either asked and were rejected (35%) or didn’t ask at all (33%) (see figures 4 and 6).
The concern is what has been reported by those who were unsuccessful in their requests. One nurse revealed to us that she was told to go back to a hospital role if she wanted a pay rise, a response that Ms Irwin describes as ‘the wrong course of action’ and one that ‘highlights poor management skills’.
Related Article: ‘Patients not prisoners’: Palliative care nursing behind bars
We also found numerous reports of GPNs offered less than the terms stated in job adverts. In particular, a case of a GPN being offered thousands below the stated salary in the advert, with the promise of a pay review six months after joining that was ultimately refused.
Ms Irwin says that our findings demonstrate why the pay deal for NHS nurses ‘must be extended to nurses working in general practice’.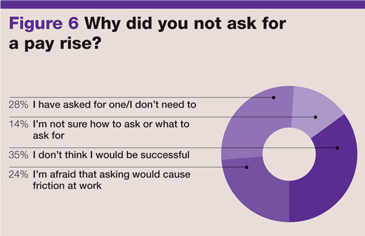
‘The pressures of an ageing workforce and nurses leaving because of poor pay means general practice is not immune to the recruitment and retention issues facing the profession. The RCN will continue to call for all staff delivering NHS services to be able to enjoy the 2018 pay deal. In the meantime, there is advice on our website [rcn.org.uk] for any practice nurses who are unsure how to initiate pay discussions with their employer.’

See how our symptom tool can help you make better sense of patient presentations
Click here to search a symptom


Practice nursing has a recruitment and retention problem, but is it any wonder when the current cohort feels so undervalued?



