Even before the onset of the Covid-19 pandemic, the social care workforce was struggling to cope. Let’s look firstly at some of the stark data: there were 1.65 million jobs (1.16 million full time equivalent) in adult social care in England in 2019/20. Though overall the workforce had been growing, registered nurses were an exception: there were 36,000, that’s 15,500 fewer than eight years previously. Over 12% of posts were vacant and four in ten nurses were leaving their posts each year.
The levels of vacancies and turnover for nurses were highest across social care and the Care Quality Commission has suggested that these workforce issues are a key factor in the relatively low quality ratings received by nursing homes.
This all suggests enormous pressure on staff. And then the pandemic struck. We know relatively little about the specific impact on nurses in social care, but we might expect it to be similar to other social care staff. The Care Quality Commission has described the intense pressure felt by social care staff and its impact on their wellbeing as the pandemic took hold.
But there were additional issues for nurses specifically within social care.
Workforce stress
Professor Martin Green, chief executive of Care England recently gave evidence to the Health and Social Care Committee on workforce burnout and resilience, stating that ‘the issues are the same in social care as in the NHS and people are dealing with similarly complex cases’.
The annual staff survey in the NHS continues to show very high levels of stress amongst nurses and midwives (44% in 2019) reporting being unwell as a result of work stress in the previous year. Essentially this is because work demands are exceeding nurses’ resources. Chronic excessive workload is a key factor and is the number one predictor of staff stress and influences nurses’ decisions to quit the profession. It manifests in emotional exhaustion, cynicism and detachment (difficulty in relating to clients as people), and distressing feelings of lack of accomplishment.
The RCN employment survey 2019 showed already excessive levels of work pressure faced by nurses across all sectors, with nearly two-thirds of those working in independent sector care homes feeling that they are under too much pressure at work. Covid-19 may have added to this. For example another RCN survey conducted in 2020 showed that 4 in 10 respondents said staffing levels had worsened during the pandemic, and this was particularly problematic in the independent and social care sectors. It is also too early to tell what the long-term consequences of the pandemic will be on staff mental health and wellbeing or how this may impact on rates of sickness absence though sickness absence during the pandemic has inevitably been high. In 2019/20 the average number of sickness days in social care was 4.7, which equates to approximately 6.72 million days lost to sickness over the 12-month period.
What should be done?
Our report for the RCN Foundation,The courage of compassion: supporting nurses and midwives to deliver high-quality care makes eight key recommendations to improve working conditions and support the wellbeing of nurses in all sectors. These apply to all sectors, though some elements will need to be adapted for the specific context of nursing within social care.
The recommendations:
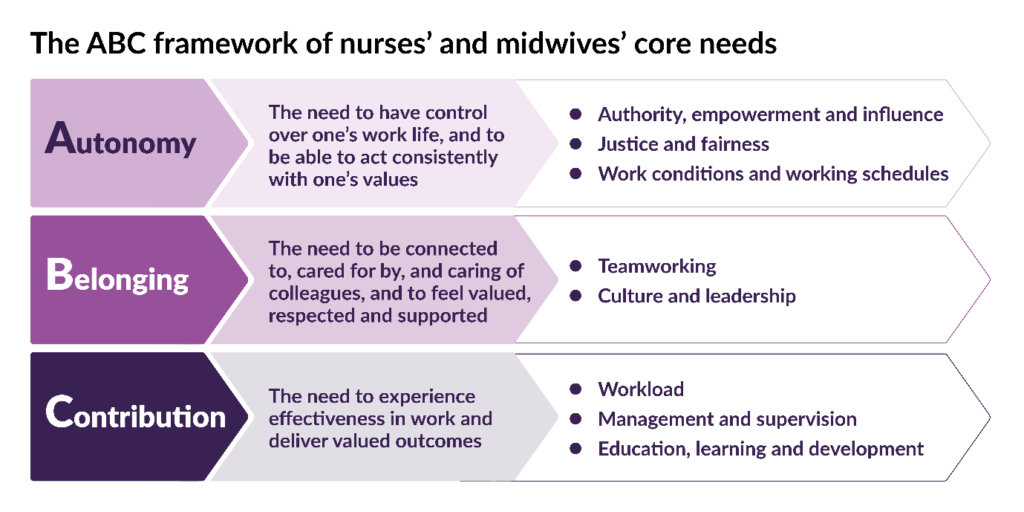
Key recommendation 1: Authority, empowerment and influence
Introduce mechanisms for social care nursing staff to shape the cultures and processes of their organisations and influence decisions about how care is structured and delivered.
Key recommendation 2: Justice and fairness
Nurture and sustain just, fair and psychologically safe cultures and ensure equity, proactive and positive approaches to diversity and universal inclusion.
Key recommendation 3: Work conditions and working schedules
Introduce minimum standards for facilities and working conditions for social care nursing staff in all organisations.
Key recommendation 4: Teamworking
Develop and support effective multidisciplinary teamworking for all social care nursing staff.
Key recommendation 5: Culture and leadership
Ensure health and care environments have compassionate leadership and nurturing cultures that enable both care and staff support to be high-quality, continually improving and compassionate.
Key recommendation 6: Workload
Tackle chronic excessive work demands in social care nursing, which exceed the capacity of nurses to sustainably lead and deliver safe, high-quality care and which damage their health and wellbeing.
Key recommendation 7: Management and supervision
Ensure all social care nursing staff have the effective support, professional reflection, mentorship and supervision needed to thrive in their roles.
Key recommendation 8: Learning, education and development
Ensure the right systems, frameworks and processes are in place for social care nurses’ learning, education and development throughout their careers. These must promote fair and equitable outcomes.
There are numerous examples across the country of where each of these recommendations is already being implemented, but they should be adopted by every care organisation across the UK. High quality, continually improving and compassionate social care can only be delivered if high quality, continually improving and compassionate support is provided for social care staff.
Everyone can help by developing and practising their teamwork skills, which lead to better social and emotional support for all team members. Our report’s ABC framework on the core needs of nurses and midwives can be used by teams to help explore workplace issues and generate ideas for local improvement.
As the pandemic has shown, the social care sector relies on the dedication of skilled and caring individuals. Social care funding reforms are long overdue but when these eventually materialise, they must be accompanied by a comprehensive, funded workforce plan. Such a plan must offer a solution to meeting the growing social care needs in our communities and protect the staff who make the difference to the lives of people across the country every day.
We are holding a free online event on 3 December, where we’ll be exploring further the essential changes in the working environments of nurses across health and social care that will enable them to flourish and thrive.






