The role of nurses in the provision of contraception in primary care

Key learning points
- All currently available LARC methods are more cost effective than the combined oral contraceptive pill even at one year of use.
- 95% of emergency contraception is the emergency pill despite the IUD being more effective and sustainable.
- It is vital for women to have access to contraception after abortion and to discuss the various methods with their nurse.
Practice nurses are ideally placed to take a prominent role in advising clients and providing them with their chosen method of contraception. Patients often raise contraception needs during consultations unrelated to contraception and assume that practice nurses will know all the answers.
Why is it important for practice nurses to play a role in contraception provision and care?
According to the Government’s Sexual Health Framework published in 2013, around 50% of all pregnancies are unplanned/unintended.1 The ambition of the Government at that time was to reduce unintended pregnancies among all women of child-bearing age through better knowledge and awareness of all methods of contraception and improve access to emergency contraception in a timely manner.
Women in Britain now spend about 30 years of their lives averting unintended/unwanted pregnancy. The third national survey of attitudes and lifestyles (NATSAL) study in 2013 stated that 16.2% of women scored their pregnancy as unplanned and 29.0% as ambivalent. The study showed that the highest risk of unplanned pregnancy was in women at the beginning and end of the family building cycle.2
Any investment in contraception makes economic sense. Unplanned or short-interval pregnancies negatively impact the health and social outcomes of women and their babies. Any effort to reduce unintended pregnancy supports Public Health England’s (PHE) Best Start in Life priority.3 It has been estimated that for every £1 invested in contraception, a savings of £11.09 is made to the national health purse.4
Due to concerns about restriction to services in some areas, a paper was published by Brook and the Family Planning Association (FPA) in 2013 titled The Unprotected Nation, which highlighted that between £3.7bn-£5.1bn could be saved by improving access to contraceptive and sexual health services.5
Raising awareness among women about all the methods of contraception and having nurses skilled to address their questions, can expel myths and help to reduce the large numbers of unintentended pregnancies. Good sexual and reproductive health is key to protecting and improving the health and wellbeing of the nation.
Related Article: NMC seeks nursing leader to oversee Code and revalidation reviews
Current commissioning arrangements for contraception, which have been in place since 2013, are somewhat fragmented with the local authority (LA) (public health) responsible for commissioning contraception provided by community services. NHS England are responsible for commissioning contraceptive services provided under the GP contract and abortion is commissioned by Clinical Commissioning Groups (CCGs). Not all CCGs commission contraception as part of abortion care. This is a missed opportunity and without clear pathways, women may not access advice or indeed get contraception for some time following abortion.
Conception rates
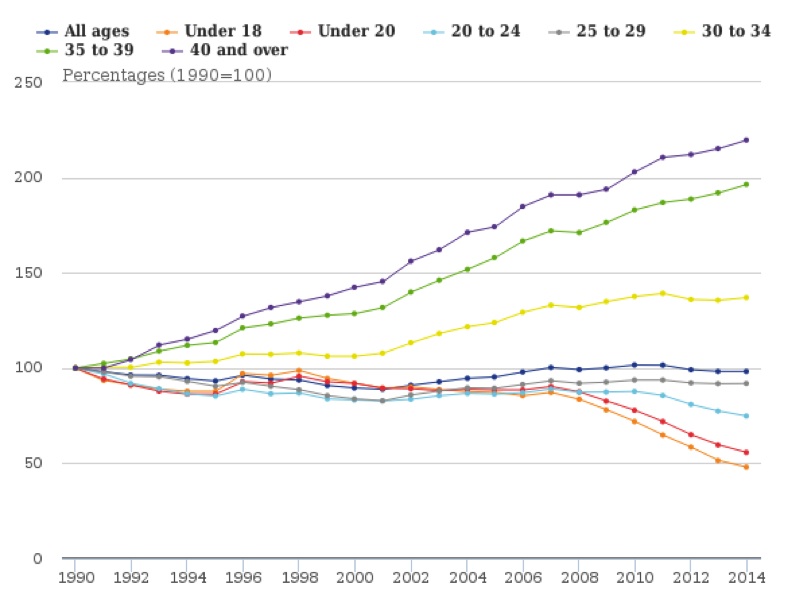
The graph below shows the conception rates by age between 1990-2014, and while conception rates are reducing among some age groups, clearly more work is needed to reduce further the unplanned rates of pregnancy.
Figure 1: Relative changes in age-specific conception rates, 1990 to 2014, England and Wales, (ONS 2016)6
Abortion data
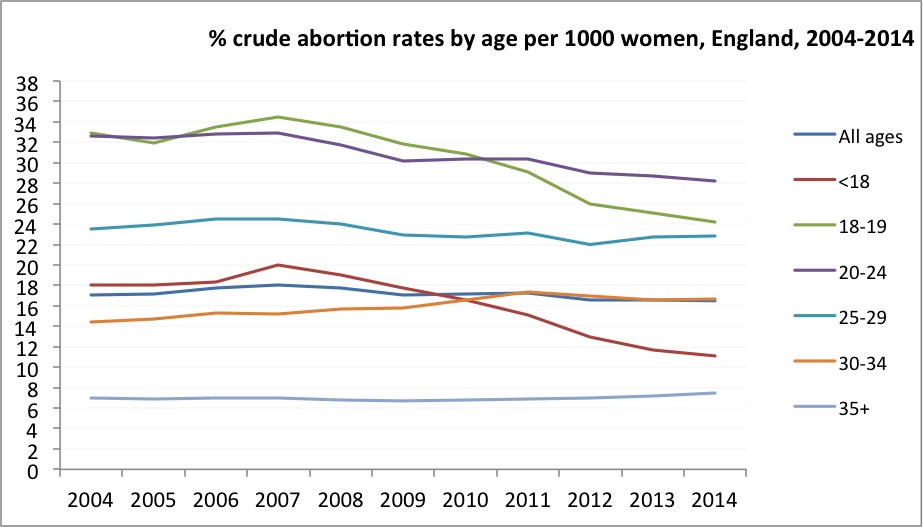
The Department of Health (DH) statistics from the graph below show that in 2014 the highest rate of abortion was among women aged 22 years at 28 per 1,000 pregnancies. Additionally in 2014, 37% of abortions were among women who had at least one other abortion. Having access to contraception after abortion is vital – some women may not be using their chosen method correctly and part of any abortion discussion and advice should be a conversation around contraceptive options. For some women this may be the first real opportunity to have a discussion with a nurse about all methods of contraception, to discuss effects and failure rates as well as the non-contraceptive benefits of some methods.
Figure 2: Crude abortion rates by age, 2004-2014, England
Methods of contraception
There are at least 15 methods of contraception available and these include:
- Combined methods (pill, ring and patch)
- Progestogen only pills (POPs)
- Intrauterine devices (copper IUD)
- Intrauterine systems (Mirena, Jaydess and Levosert)
- Subdermal implants (Nexplanon)
- Condoms (male and female)
- Sterilisation (male and female)
- Diaphragms
- Natural fertility awareness
- Lactation amenorrhoea
The most effective methods of contraception are long-acting reversible contraceptives (LARC). NICE 8 published the first ever guidance on LARC in 2005. The four methods are IUDs, intrauterine systems (IUS) subdermal implants (SDI) and injectables. NICE highlighted in the guidance that:
- All currently available LARC methods are more cost effective than the combined oral contraceptive pill, even at one year of use.
- The IUS and implants are more cost effective than the injectable contraceptives.
- Increasing the uptake of LARC methods should help reduce the numbers of unintended pregnancies.
In September 2016 NICE9 published a new quality standard that set out the key areas where advice to women on contraception needs to improve. It is estimated by NICE that in 2014/15 some 95% of emergency contraception supplied by sexual and reproductive health services was the emergency pill, despite the fact that the IUD is more effective and women may wish to continue using it as their chosen method.
Despite the recommendations of NICE in 2005 and again in 2016 that LARC are more effective, many women still experience restrictions to access to the full range of contraceptive methods and the most effective emergency contraceptive method.
Related Article: Tell us what practice nursing means to you and potentially win £1,000
For example, intrauterine contraception is safe, highly effective and, in line with all other methods of contraception, is free to women in the UK. It was estimated that only 9% of women attending community contraceptive clinics during 2014-2015 were using intrauterine methods (4% were using the intrauterine device (IUD) and 5% using the intrauterine system (IUS).10
The reasons for low use of LARC are varied and include:
- Lack of awareness of LARC among women and therefore they do not ask about them.
- Lack of knowledge about LARC among health professionals.
- Lack of training opportunities for nurses to provide LARC, therefore if unable to offer LARC is not mentioned.
- Time needed to train and gain competency to fit IUDs and insert SDIs may prohibit nurses from advancing their practice.
What training and education do practice nurses need to deliver a comprehensive contraceptive service?
It must be acknowledged that practice nurses cannot be expected to deliver a service if they are not adequately skilled and familiar with the most up-to-date clinical guidelines and national standards on contraception and sexual health. The current pressures on reduced budgets for training make it more difficult for nurses to access this. Traditionally, the nursing universities provide programmes in contraception and sexual health but these involve time away from work and can be costly.
Education and training must be viewed as a fundamental aspect of effective and sustainable health service planning and delivery, ensuring that patients continue to receive the highest standards of care. Education and training should be a mandatory inclusion in all commissioned contracts. The local education and training boards (LETBs) could take a lead on ensuring that local training needs assessments are done to ensure that staff with the right knowledge and skills are in place to deliver the service.
Many nurses miss the opportunity for contraception and sexual health skills acquisition during the nurse pre-registration programme because there may be a lack of experts on sexual health to deliver the programmes. Once qualified some nurses may have difficulty in accessing programmes due to cost and time away from work.
More recently, the Faculty of Sexual and Reproductive Healthcare (FSRH) have opened their programmes to nurses with doctors and nurses undertake the same training. The FSRH recently developed an essential skills programme, known as SRH essentials. This is a one-day interactive course for nurses working in primary care. The programme has been rolled out across the four countries. For venues, dates and contact details see link below to the FSRH training programme.11
Practice nurses who would like to develop skills in the insertion of subdermal implants and intrauterine devices/systems are now able to gain competencies through the FSRH. The FSRH provide an online course for skills acquisition related to sexual and reproductive healthcare, which is available for a modest fee. Nurses considering this route should in the first instance read all the FSRH guidelines related to each method of contraception, including the United Kingdom Medical Eligibility Criteria (UKMEC).12 The UKMEC was updated in 2016 and gives clear guidance on which methods should not be used by women with specific conditions. Nurses can apply to undertake the FSRH electronic knowledge assessment (eKA) test which must be completed before any clinical training can take place.
The key to success with the eKA is to spend some time reading all the guidelines before considering taking the test, as the questions from the random eKA test will be covered in the guidance and they should not undertake the eKA until they feel confident they will pass. They can re-take the test but will need to pay each time. Colleagues recommend good preparation and then a quiet time to do the test without interruption.
Related Article: MPs vote to legalise assisted dying in England and Wales
Nurses who complete the electronic module can then apply to be trained by a FSRH trainer who holds the letter of competence (LoC) and once competent the nurse will be awarded a LoC for either subdermal implants or intrauterine techniques. This is the national gold standard for training and most commissioners now insist on it when they commission services. The FSRH guidance on training stipulates ongoing maintenance of competency and updating.
Any nurse, regardless of place of practice, who has a role in contraception advice and provision should be familiar with the UKMEC. The UKMEC was updated in May 2016 and there are some changes to all methods of contraception. All the guidelines are available at www.fsrh.org.13
References
- Department of Health. A framework for sexual health improvement in England. London: DH; 2013
- British National Surveys of Sexual Attitudes and Lifestyles. National survey of sexual attitudes and lifestyles 3 (NATSAL). The Lancet: 2013; 382:1757-1856
- Public Health England. Best start in life and beyond: Improving public health outcomes for children, young people and families. PHE: 2016
- Bayer HealthCare. Care Contraception Atlas. Bayer HealthCare: 2013
- Lucas S. The unprotected nation: The Financial and economic Impact of restricted contraceptive and sexual health services. London: FPA; 2013
- Office of National Statistics. Conception and fertility rates. London: ONS; 2016
- Office of National Statistics. Abortion statistics, England and Wales, 2014. London: ONS; 2016
- NICE. CG30: Long acting reversible contraception. London: NICE; 2005
- NICE. Coil is more effective than the pill as emergency contraception. London: NICE; 2016
- Walker. S, Newton, V, Hoggart, L and Parker, M Predictors of non-use of intrauterine contraception among women aged 18-49 years in a general practice setting in the UK. Open Access Journal of Contraception 2016:7 155-160
- Faculty of Sexual and Reproductive Healthcare. Careers and training essentials. London: FSRH; 2016
- Faculty of Sexual and Reproductive Healthcare. Careers and training e-knowledge assessment. London: FSRH; 2016
- Faculty of Sexual and Reproductive Healthcare. United Kingdom Medical Eligibility Criteria. London: FSRH; 2016

See how our symptom tool can help you make better sense of patient presentations
Click here to search a symptom


Practice nurses are ideally placed to take a prominent role in advising clients and providing them with their chosen method of contraception.



